Hybrid Models of Care
At the beginning of the COVID-19 pandemic, healthcare professionals rapidly shifted to the use of telehealth. This was especially true for psychiatrists, with many transitioning to telepsychiatry. This helped them to avoid having their patients come into an office setting, mitigating the spread of COVID-19. According to two surveys completed by APA among a sample of its membership, at the height of the pandemic, psychiatrists were using telepsychiatry (meaning both live videoconferencing and audio-only options) with over 90% of their patients. However, as more people are vaccinated against COVID-19, and as cases continue to drop, many psychiatrists are wondering where telepsychiatry might fit in to their practice.
One option, known as “hybrid care,” incorporates telepsychiatry and other health technologies with traditional in-person care. In this model, the psychiatrist-patient relationship is mediated through commonly used communications technologies (telephone, e-mail, video) in conjunction with clinical support technologies (e.g., electronic health record systems, e-prescribing), while still offering in-person appointments. In short, a hybrid model maximizes the benefits of using a virtual space in conjunction with the traditional familiarity of a physical space.
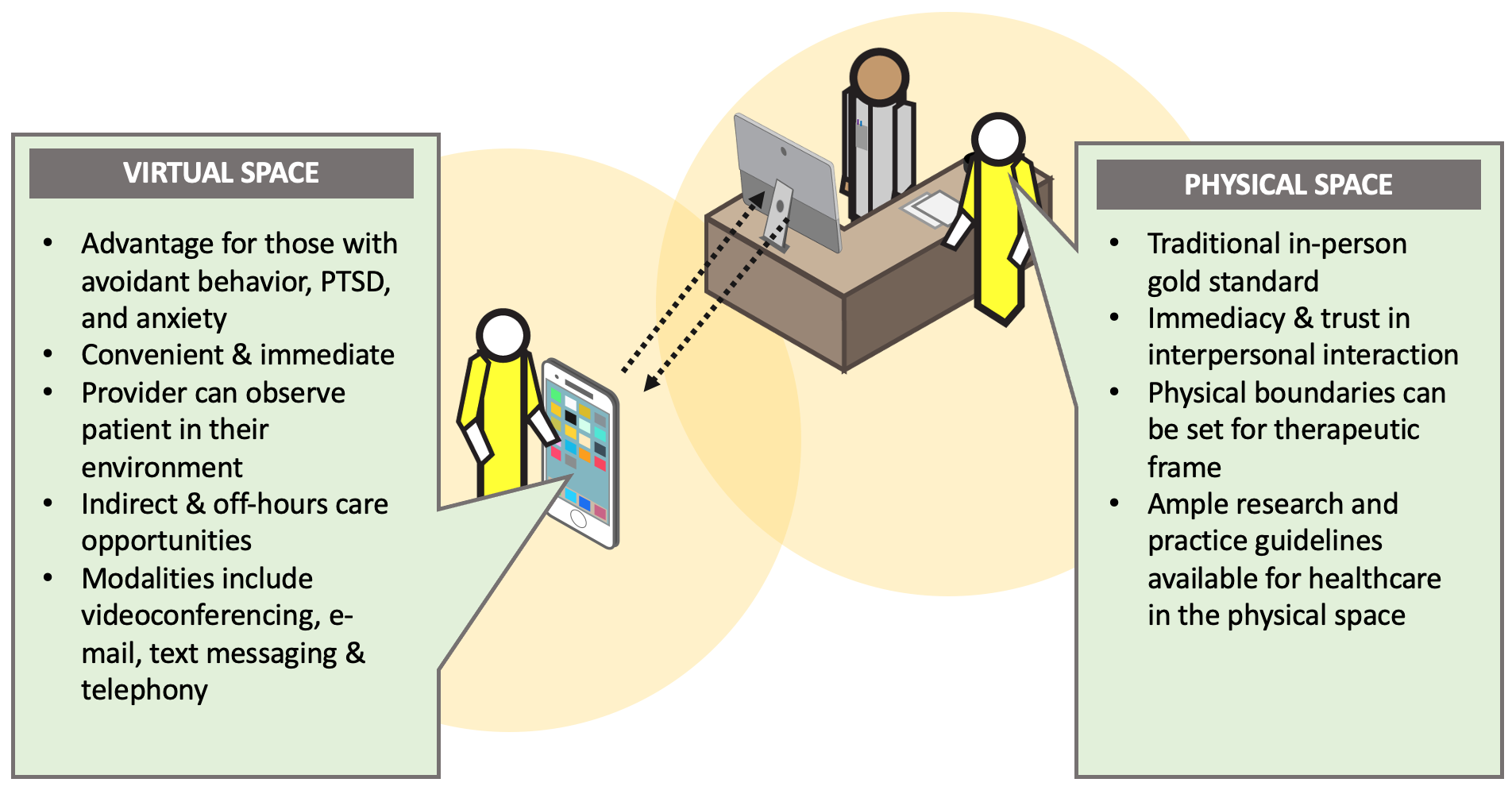
*Image Text*
Header: Hybrid Model of Care
Subheader: Virtual Space
Unordered List:
- Advantage for those with avoidant behavior, PTSD, and anxiety
- Convenient & immediate
- Provider can observe patient in their environment
- Indirect & off-hours care opportunities
- Modalities include videoconferencing, e-mail, text messaging & telephony
Subheader: Physical Space
Unordered List:
- Traditional in-person gold standard
- Immediacy & trust in interpersonal interaction
- Physical boundaries can be set for therapeutic frame
- Ample research and practice guidelines available for healthcare in the physical space
*End Image Text*
While a hybrid model of care offers both strengths and limitations to the psychiatrist-patient therapeutic relationship, there are three core considerations when evaluating whether the hybrid model is a good fit for any practice: Administrative, Operational, and Clinical. Administrative considerations include issues like legal, regulatory, and technology requirements. Operational include how to successfully integrate technology in a practice setting. Clinical involves the impact of the use of technology on the clinical process.
APA has developed a new resource, Hybrid Psychiatrist-Patient Relationships: Proficiencies for 21stCentury Psychiatry, for you to use as you evaluate whether adopting a hybrid model into your practice is a good fit. APA also plans on adding other resources on hybrid models of care to its Telepsychiatry Toolkit in the near future—but be sure to check-out our recent blogs on using telepsychiatry during the COVID-19 Public Health Emergency.
