There are many complex connections between skin conditions and mental health conditions. Psychodermatology is the subspecialty that addresses these connections. A recent Special Section in Psychiatric News, authored by Mohammad Jafferany, M.D., professor of psychodermatology, psychiatry, and behavioral sciences at Central Michigan University College of Medicine, addressed it.
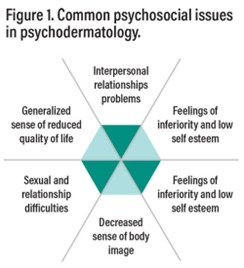
More than one-third of dermatological patients have psychological concerns. Psoriasis, atopic dermatitis, and eczema are among the skin diseases most associated with co-occurring mental health conditions. People with chronic skin conditions, such as psoriasis or vitiligo, can experience low self-esteem, concerns with body image and social isolation. (See figure 1.) These issues can impact a person’s social interactions, employment, quality of life and overall mental well-being.
Public misperceptions (that chronic conditions are contagious, for example), and stigma associated with skin conditions can add emotional distress. These factors contribute to higher rates of depression and anxiety among people with chronic dermatologic conditions. Patients’ personality traits and life circumstances also influence how they perceive their skin disease. People with obsessive-compulsive traits, for example, may be more prone to skin-picking.
Psychodermatological disorders include both mental health disorders affecting skin and skin disorders linked with mental health conditions. Types of conditions include
- Skin conditions made worse by psychological stress, such as psoriasis, atopic dermatitis, and rosacea.
- Primary psychiatric disorders: Conditions in which skin problems are a symptom of the disorder, such as hair-pulling disorder (trichotillomania) and skin picking disorder (excoriation).
- Emotional problems caused by having a visible skin disease, such as vitiligo, psoriasis, and alopecia areata.
- Unpleasant skin sensations, such as itching, burning, or stinging, without a clear dermatological or psychiatric diagnosis.
In addition, mental health medications may cause dermatological side effects, and many dermatological medications may cause psychiatric side effects. (See Table 2 in the Psychiatric News Special Section for a list of side effects.)
An example of the complexity of the relationship is atopic dermatitis, a skin condition resulting in rashes and itchy skin. In early infancy, it can interfere with bonding between mother and child. Babies with atopic dermatitis may not be able to tolerate being held and may be irritable, which may be difficult for parents and other caregivers. Children with atopic dermatitis may experience social isolation and parents may have feelings of helplessness. Older children and teens may experience bullying and difficulties with some social and sporting activities.
A comprehensive, multidisciplinary approach to addressing these complex psychodermatological disorders is crucial to improving the quality of life for patients, per Jaffanery’s artilce. The approach should include psychological assessment and treatment along with treatment of skin condition(s). Treatment often involves a combination of psychotropic medications, such as selective serotonin reuptake inhibitors (SSRIs) for depression and anxiety, and cognitive behavioral therapy which has proven effective in treating behaviors like skin-picking and trichotillomania.
References
- Jafferany, M. 2025. Special Report: Psychodermatology: Bridging Dermatology and Psychiatry. Psychiatric News, Volume 60, Number 3, https://doi.org/10.1176/appi.pn.2025.03.3.2
