Eating Disorders, Weight-Shaming and “Clean” Eating
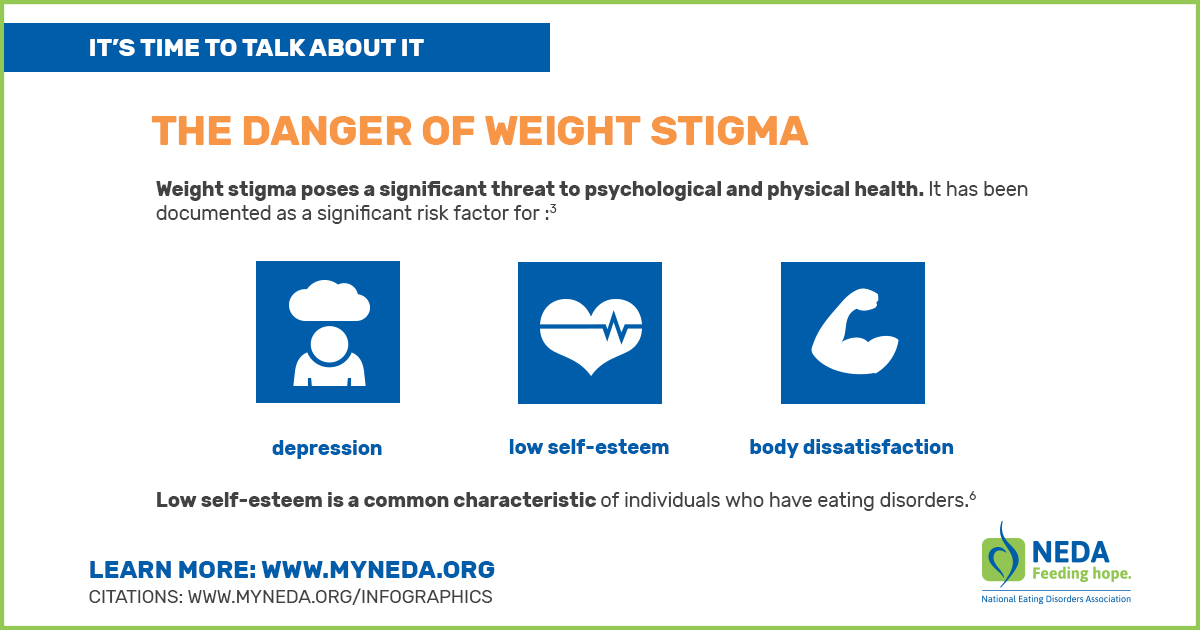
Eating disorders affect all kinds of people: women, men, young and old and from all racial and ethnic backgrounds. Many factors likely contribute to developing eating disorders, including a range of biological, psychological, and sociocultural factors. Having a close relative with an eating disorder or a history of dieting are risk factors. High levels of body image dissatisfaction and setting unrealistically high expectations for oneself (perfectionism) also increase the risk. Experiencing teasing or bullying about weight or weight stigma (discrimination or stereotyping based on weight) also increase a person’s risk for eating disorders.
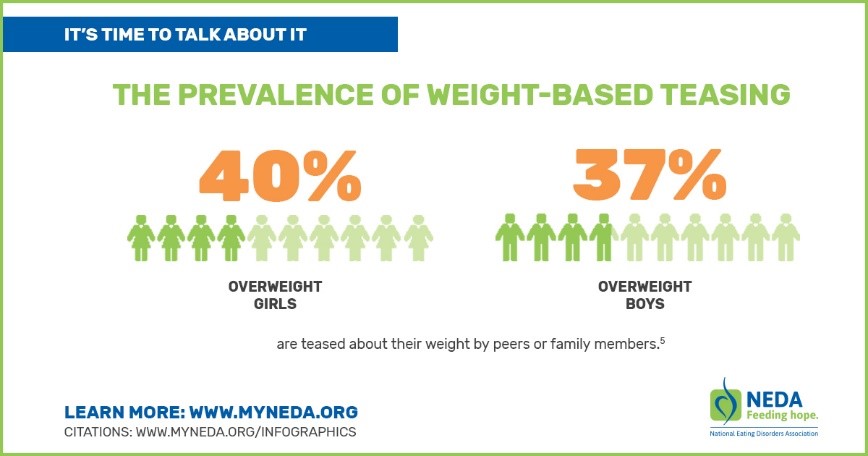 The best-known environmental contributor developing an eating disorder is the cultural idealization of thinness. Media portrayals of the perfection of thin are pervasive. Nearly 40 percent of overweight girls and boys are teased about their weight by peers or family members. Weight teasing is associated with weight gain, binge eating, and extreme weight control measures. The National Eating Disorders Association offers a quiz--a reality check about what people are saying and what you're hearing about food and body image issues. Take the Quiz.
The best-known environmental contributor developing an eating disorder is the cultural idealization of thinness. Media portrayals of the perfection of thin are pervasive. Nearly 40 percent of overweight girls and boys are teased about their weight by peers or family members. Weight teasing is associated with weight gain, binge eating, and extreme weight control measures. The National Eating Disorders Association offers a quiz--a reality check about what people are saying and what you're hearing about food and body image issues. Take the Quiz.
A large study of adolescents (14 and 15 years old) found that dieting was an important predictor of a developing eating disorder. Those who dieted moderately were 5x more likely to develop an eating disorder than those who did not diet. One third or more of adolescent girls engage in unhealthy weight-control behaviors, such as crash dieting, skipping meals or fasting, self-induced vomiting or taking diet pills or laxatives. Even among clearly non-overweight girls, more than one-third report dieting.
 A recent area of concern is the popularity of “clean eating”—a focus on eating whole, natural, unprocessed foods and avoiding artificial ingredients and processed and packaged foods. While this type of eating can be generally healthy, an extreme focus and overly restrictive eating can be problematic. This type of restriction and focus is not a separate disorder identified in the Diagnostic and Statistical Manual of Mental Disorders (DSM), but is a recognized condition called orthorexia. (See a previous blog on Orthorexia.)
A recent area of concern is the popularity of “clean eating”—a focus on eating whole, natural, unprocessed foods and avoiding artificial ingredients and processed and packaged foods. While this type of eating can be generally healthy, an extreme focus and overly restrictive eating can be problematic. This type of restriction and focus is not a separate disorder identified in the Diagnostic and Statistical Manual of Mental Disorders (DSM), but is a recognized condition called orthorexia. (See a previous blog on Orthorexia.)
Starting a Conversation
If you’re worried about a loved one, here are some tips on starting a conversation.
- Express your concerns honestly, respectfully and in a loving supportive way.
- Talk to your loved one about specific things you see or feel. Share memories of times you were concerned about their eating or exercise rituals. • Use “I” statements, such as “I’m concerned when I see….”
- Avoid accusatory “You” statements, such as “You’re out of control!” • Avoid giving simple solutions, such as “If you’d just stop then everything would be fine.”
(Source: National Eating Disorders Association)
Getting Help for Disordered Eating
National Association of Anorexia Nervosa and Associated Disorders, Inc.
Helpline: 630-577-1330
Help is also available through support groups.
Overeaters Anonymous
Helpline: 505-891-2664
Help is available through in person, online and phone-based support groups: find a meeting. Overeaters Anonymous is not just for people who are concerned about eating too much; it is also for those who have anorexia, bulimia, food addiction, or any other type of eating disorder.
National Eating Disorders Association
Helpline: 1-800-931-2237
Support, information, referrals, and guidance about treatment options are also available through online chat and text.
References
- Andreveva, T., Puhl, R. M. and Brownell, K. D. (2008), Changes in Perceived Weight Discrimination Among Americans, 1995–1996 Through 2004–2006. Obesity, 16: 1129–1134.
- Culbert, K. M., Racine, S. E., & Klump, K. L. (2015). Research Review: What we have learned about the causes of eating disorders - a synthesis of sociocultural, psychological, and biological research. J Child Psychol Psychiatry, 56(11), 1141-1164.
- Golden, N. H., Schneider, M., & Wood, C. (2016). Preventing Obesity and Eating Disorders in Adolescents. Pediatrics, 138(3).
- Hatzenbuehler ML, Keyes KM, Hasin DS. Associations between perceived weight discrimination and the prevalence of psychiatric disorders in the general population. Obesity 2009;17(11)2033–2039.
- Neumark-Sztainer, D. (2005). I’m, Like, SO Fat!.New York: Guilford. • Neumark-Sztainer, D., &Hannan, P. (2001). Weight-related behaviors among adolescent girls and boys: A national survey. Archives of Pediatric and Adolescent Medicine, 154, 569-577.
- Wertheim, E., Paxton, S., &Blaney, S. (2009). Body image in girls.In L. Smolak & J. K. Thompson (Eds.), Body image, eating disorders, and obesity in youth: Assessment, prevention, and treatment (2nd ed.) (pp. 47-76). Washington, D.C.: American Psychological Association.
